Information about Asthma Inhalers
The most common symptoms of asthma are:
- Wheezing (a whistling sound when breathing)
- Breathlessness
- A tight chest - which may feel like a band is tightening around it
- Coughing
- Happen often and keep coming back
- Are worse at night and early in the morning
- Seem to occur in response to an asthma trigger - for example, exercise or exposure to an allergen (such as pollen or animal fur)
- Wheezing, coughing and chest tightness becoming severe and constant
- Being too breathless to eat, speak or sleep
- Breathing faster
- A rapid heartbeat
- Drowsiness, confusion, exhaustion or dizziness
- Blue lips or fingers
- Fainting
- A family history of asthma or related allergic conditions (known as atopic conditions) such as eczema, food allergy or hay fever
- Having another atopic condition yourself
- Having bronchiolitis (a common childhood lung infection) as a child
- Exposure to tobacco smoke as a child
- Your mother smoking during pregnancy
- Being born prematurely or with a low birth weight
- Some people may also be at risk of developing asthma through their job.
- Infections - particularly infections of the upper airways, such as colds and flu
- Allergens - including pollen, dust mites, animal fur ("dander") or feathers
- Airborne irritants - including cigarette smoke, fumes and pollution
- Medicines - particularly painkillers called non-steroidal anti-inflammatory drugs (NSAIDs), which include aspirin and ibuprofen, and beta-blockers
- Emotions - including stress or laughter
- Food additives - including sulphites (often found in pickled products, wine, beer and dried fruit) and tartrazine (a yellow food colouring)
- Weather conditions - including sudden changes in temperature, cold air, windy days, thunderstorms and hot, humid days
- Indoor conditions - including mould or damp and chemicals in carpets and flooring materials
- Exercise
- Food allergies - including allergies to nuts and other foods
- Mild shaking of the hands (tremors)
- Headaches
- Muscle cramps
- A fast, pounding or fluttering heartbeat (palpitations)
- A fungal infection of the mouth or throat (oral thrush)
- A hoarse voice
- A sore throat
- Leukotriene receptor antagonists - taken once a day to stop the airways becoming inflamed (syrup and powder forms are also available)
- Theophyllines - taken twice a day to help widen the airways
- Steroid tablets - see below
- As an immediate, short-term treatment if you have occasional severe asthma attacks
- As a long-term treatment if other medications don't control your symptoms well enough
- Osteoporosis (fragile bones)
- High blood pressure
- Diabetes
- Increased appetite, leading to weight gain
- Cataracts and glaucoma
- Thinning of the skin
- Easy bruising
- Muscle weakness, especially around the thighs and shoulders
- Mood changes
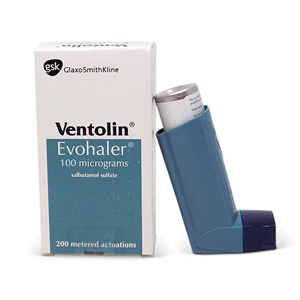
- Pressurised canisters - you press the inhaler while breathing in and it releases a spray of medicine into your lungs (these are sometimes used with a device called a spacer - see below)
- Dry powder inhalers - non-pressurised devices that release powdered medication when you breathe in quickly and forcefully
- they can make inhalers more effective because more of the medicine reaches the lungs
- less medicine stays in the mouth or is swallowed, so problems such as oral thrush are less likely to occur
- they're easier to use for children who may otherwise find it difficult to use an inhaler correctly
- a face mask can be attached to the mouthpiece to make it easier for very young children to breathe in the medicine
- Make sure the people you are exercising with know you have asthma
- Always have your reliever inhaler with you when you exercise
- Use your reliever inhaler immediately before you warm up
- Ensure that you always warm up and down thoroughly
- talking about your symptoms - such as whether they're affecting your normal activities or are getting worse
- a discussion about your medication - including whether you think you might be experiencing any side effects and whether you need to be reminded how to use your inhaler correctly
- breathing tests
- Keep warm and dry - wear gloves, a scarf and a hat, and carry an umbrella.
- Wrap a scarf loosely over your nose and mouth - this will help to warm up the air before you breathe it in.
- Try breathing in through your nose instead of your mouth as your nose warms the air as you breathe in.
- Your symptoms may get worse during pregnancy (although some women find they improve), so your treatment may need to be reviewed regularly
- Poorly controlled asthma in pregnancy can increase the risk of complications such as pre-eclampsia, premature birth and restricted growth of the baby in the womb
- Extra precautions may need to be taken during labour to avoid an asthma attack (although attacks during labour are rare)
Chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease (COPD) is the name for a group of lung conditions that cause breathing difficulties.
It includes:
- Emphysema - damage to the air sacs in the lungs
- Chronic bronchitis - long-term inflammation of the airways
- Increasing breathlessness, particularly when you're active
- A persistent chesty cough with phlegm - some people may dismiss this as just a "smoker's cough"
- Frequent chest infections
- Persistent wheezing
- Stopping smoking - if you have COPD and you smoke, this is the most important thing you can do
- Inhalers and medications - to help make breathing easier
- Pulmonary rehabilitation - a specialised programme of exercise and education
- Surgery or a lung transplant - although this is only an option for a very small number of people
- Increasing breathlessness - this may just occur when exercising at first, and you may sometimes wake up at night feeling breathless
- A persistent chesty cough with phlegm that never seems to go away
- Frequent chest infections
- Persistent wheezing
- Weight loss
- Tiredness
- Swollen ankles from a build-up of fluid (oedema)
- Chest pain and coughing up blood - although these are usually signs of another condition, such as a chest infection or possibly lung cancer
- Cadmium dust and fumes
- Grain and flour dust
- Silica dust
- Welding fumes
- Isocyanates
- Coal dust
- Ask about your symptoms
- Examine your chest and listen to your breathing with a stethoscope
- Ask whether you smoke or used to smoke
- Calculate your body mass index (BMI) using your weight and height
- Ask if you have a family history of lung problems
- An electrocardiogram (ECG) - a test that measures the electrical activity of the heart
- An echocardiogram - an ultrasound scan of the heart
- A peak flow test - a breathing test that measures how fast you can breathe out, which can help rule out asthma
- A blood oxygen test - a peg-like device is attached to your finger to measure the level of oxygen in your blood
- A computerised tomography (CT) scan - a detailed scan that can help identify any problems in your lungs
- A phlegm sample - a sample of your phlegm (sputum) may be tested to check for signs of a chest infection
- beta-2 agonist inhalers - such as salbutamol and terbutaline
- antimuscarinic inhalers - such as ipratropium
- beta-2 agonist inhalers - such as salmeterol, formoterol and indacaterol
- antimuscarinic inhalers - such as tiotropium, glycopyronium and aclidinium
- weight gain
- mood swings
- weakened bones (osteoporosis)
- Coughing up yellow or green phlegm
- A high temperature (fever)
- A rapid heartbeat
- Chest pain or tightness
- Feeling confused and disorientated
- Physical exercise training tailored to your needs and ability - such as walking, cycling and strength exercises
- Education about your condition for you and your family
- Dietary advice
- Psychological and emotional support
- Dusty places
- Fumes, such as car exhausts
- Smoke
- Air freshener sprays or plug-ins
- Strong-smelling cleaning products (unless there's plenty of ventilation)
- Hairspray
- Perfume
- Talking about your symptoms - such as whether they're affecting your normal activities or are getting worse
- A discussion about your medication - including whether you think you might be experiencing any side effects
- Tests to monitor your health
- Relaxed, slow, deep breathing
- Breathing through pursed lips, as if whistling
- Breathing out hard when doing an activity that needs a big effort
- Paced breathing, using a rhythm in time with the activity, such as climbing stairs
What can I expect from asthma treatment?
The aim of asthma management is to control of the disease, which means symptoms are well-controlled and have little to no impact on daily life. Complete control is defined as:
o No daytime symptoms.
o No night-time waking due to asthma.
o No need for rescue medication.
o No asthma attacks.
o No limitations on activity including exercise.
o Normal lung function (FEV1 and/or PEF > 80% predicted or best).
o Minimal side-effects from medication.
1. If you have asthma you should have a review of your symptoms every year, to see if any adjustments need to be made to your treatment. This can be done through your own surgery or by speaking to one of our doctors [here]. You can take the Asthma Control Test to see how well controlled your symptoms are. [link]
2. Getting your inhaler technique right is very important to ensure the medication reaches the right part of your lungs. Asthma UK has some useful videos to help you check your technique
3. A personalised action plan can help you stay in control of your asthma. Asthma UK has a template which you can talk through with a doctor [click here to book an appointment]
4. If you have asthma you are entitled to a free annual flu vaccination. This is important in protecting you from catching flu which could make your breathing worse
5. It is helpful to understand the things that trigger your asthma or make it worse, such as air pollution, smoke, pollen and other allergens or medications such as beta blockers and NSAIDs (e.g. aspirin/ibuprofen)
6. Stopping smoking is really important if you have asthma. Our doctors can help you with this or see www.smokefree.gov
7. If you are overweight, losing weight can also help with your breathing.
8. If you feel your asthma is getting you down or making you feel anxious, we can help. Talk to one of our doctors or your own GP for further advice.
1. If you have COPD you should have a review of your symptoms every year, to see if any adjustments need to be made to your treatment. This can be done through your own surgery or by speaking to one of our doctors [here]. You can take the COPD assessment test to see how well your symptoms are controlled [link to COPD assessment test]
2. Stopping smoking is really important if you have COPD. Our doctors can help you with this or see www.smokefree.gov
3. If you have COPD you are entitled to a free annual flu vaccination. This is important in protecting you from catching flu which could make your breathing worse or lead to a serious chest infection
4. Getting your inhaler technique right is very important to ensure the medication reaches the right part of your lungs. Asthma UK has some useful videos to help you check your technique
5. A personalised action plan can help you stay in control of your COPD. Asthma UK has a template which you can talk through with a doctor [click here to book an appointment]. It often involves having a ‘rescue pack’ of antibiotics and steroids at home and knowing when to use them to nip a chest infection in the bud
6. If you are overweight, losing weight can also help with your breathing.
7. It is helpful to understand the things that make your COPD worse, such as air pollution, smoke, pollen and other allergens or medications such as beta blockers and NSAIDs (e.g. aspirin/ibuprofen)
8. Evidence shows that people with long-term health conditions such as COPD are more likely to experience low mood, depression and anxiety. If you feel your condition is getting your down, we can help. Book an appointment with a doctor today.
Treatment Options
How Our Service Works
1
Register and complete
your online consultation
your online consultation
2
Select your treatment to
be collected from your
nearest pharmacy or delivered.
be collected from your
nearest pharmacy or delivered.
3
Our Doctors will assess
your suitability for treatment
your suitability for treatment
4
If approved, prescription is sent electronically to your
nominated pharmacy to allow
you to start treatment.
nominated pharmacy to allow
you to start treatment.